What Is A Meningioma
Meningiomas are the most common benign intracranial tumor. They originate from arachnoid cap cells, which are cells within the thin, spider web-like membrane that covers the brain and spinal cord. The arachnoid is one of three protective layers, collectively known as the meninges, surrounding the brain and the spinal cord. The meninges also include the dura mater and pia mater. Although the majority of meningiomas are benign, these tumors can grow slowly until they are very large if left undiscovered and, in some locations, can be severely disabling and life-threatening. Most patients develop a single meningioma; however, some patients may develop several tumors growing simultaneously in other parts of the brain or spinal cord.Types of Menigiomas
- Cavernous Sinus Meningioma: Occurs near the area that drains deoxygenated blood to the heart from the brain.
- Cerebellopontine Angle Meningioma: Located near the margin of the cerebellum; acoustic neuromas (vestibular schwannoma) typically are found in this area.
- Cerebral Convexity Meningioma: Located on the upper surface of the brain cerebral convexity.
- Foramen Magnum Meningioma: Located near the opening at the base of the skull through which the lower portion of the brainstem passes.
- Intraorbital Meningioma: Located in or around eye sockets.
- Intraventricular Meningioma: Located in the chambers through which cerebrospinal fluid is carried throughout the brain.
- Olfactory Groove Meningioma: Located along the nerves connecting the nose to the brain.
- Parasagittal/Falx Meningioma: Located adjacent to the dural fold that separates the two brain hemispheres
- Petrous Ridge Meningioma: Portion of the temporal bone (which supports the temple) that contain sections of the organs that facilitate hearing.
- Posterior Fossa Meningioma: Occurs near the back of the brain.
- Sphenoid Meningioma: Located near the sphenoid bone behind the eyes.
- Spinal Meningioma: Located in the spine, in some cases against the spinal cord.
- Suprasellar Meningioma: Located near the area of the skull where the pituitary gland is found.
- Tentorium Meningioma: Located near where the brain connects to the brainstem, an area known as the tentorium cerebelli.
Prevalence and Incidence:
According to the Brain Science Foundation and the American Society of Clinical Oncology, meningiomas account for about 34 percent of all primary brain tumors and most often occur in people between the ages of 30 and 70. Malignant meningiomas account for about two to three percent of all meningiomas.
Risk Factors
As noted earlier, meningiomas most often occur in people between the ages of 30 and 70. Children are not as likely as adults to develop meningioma.
Women are more than two times as likely as men to develop a meningioma. Malignant meningioma diagnoses are three times as likely in men. Spinal meningiomas occur 10 times more frequently in women than in men.
Exposure to ionizing radiation, especially high doses, has been associated with a higher incidence of intracranial tumors, particularly meningiomas. There also is evidence indicating a connection between meningiomas and low doses of radiation. The most well-known case involves children in Israel who were given radiation for scale ringworm between 1948 and 1960. Within the U.S., dental X-rays are the most common form of exposure to ionizing radiation. A number of studies have linked the number of full mouth dental radiographs to increased risk of meningioma.
The genetic disorder Neurofibromatosis type 2 (NF2) is believed to put people at a higher risk of developing meningioma. Patients with NF2 also may be more likely to develop malignant or multiple meningiomas.
Per the Brain Science Foundation, a number of studies have suggested a correlation between meningiomas and hormones. Such findings include the following:
• Increased occurrence of meningioma in women
• The detection of such hormones as estrogen, progesterone and androgen in some meningiomas
• A link between breast cancer and meningioma
• A connection between meningioma growth, menstrual cycles and pregnancy
Researchers are beginning to explore the possible connection between meningioma risk and the use of oral contraceptives and hormone-replacement therapy procedures.
Types and Classification
The World Health Organization (WHO) classification of brain tumors is the most widely utilized tool in grading tumor types. The WHO classification scheme recognizes 15 variations of meningiomas according to their cell type as seen under a microscope. These variations are called meningioma subtypes; the technical term for these cell variations is histological subtypes.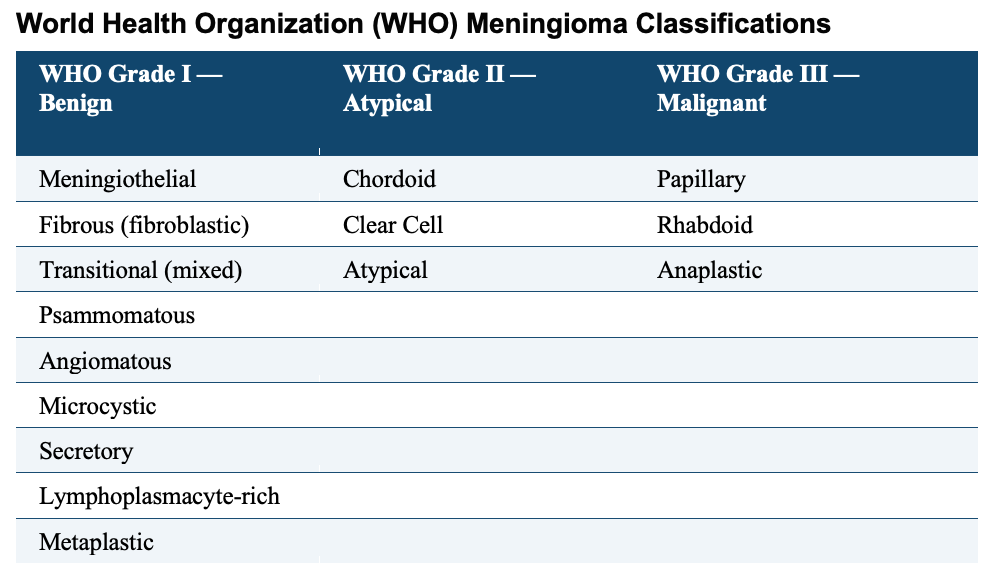
Atypical meningiomas (which account for seven to eight percent of meningioma cases) exhibit increased tissue and cell abnormalities. These tumors grow at a faster rate than benign meningiomas and can invade the brain. Atypical meningiomas have a higher likelihood of recurrence than benign meningiomas.
Malignant meningiomas show increased cellular abnormalities, and grow at a faster rate than benign and atypical meningiomas. Malignant meningiomas are the most likely to invade the brain, spread to other organs in the body and recur more often than the other two types.
Symptoms
Because meningiomas commonly are slow-growing tumors, they often do not cause noticeable symptoms until they are quite large. Some meningiomas may remain asymptomatic for a patient’s lifetime or be detected unexpectedly when a patient has a brain scan for unrelated symptoms. Presenting signs and symptoms depend on the size and location of the tumor. Symptoms of meningiomas may include any of the following:
• Headaches
• Seizures
• Change in personality or behavior
• Progressive focal neurologic deficit
• Confusion
• Drowsiness
• Hearing loss or ringing in the ears
• Muscle weakness
• Nausea or vomiting
• Visual disorders
Symptoms can be related more specifically to the location of the meningioma. Examples include the following:
• Falx and Parasagittal: Impaired levels of brain functioning such as reasoning and memory. If located in the middle section, it would likely cause leg weakness/numbness or seizures.
• Convexity: May cause seizures, headaches and neurological deficits.
• Sphenoid: Vision problems, loss of sensation in the face or facial numbness and seizures
• Olfactory Groove: Loss of smell due to compression of the nerves that run between the brain and the nose. If the tumor grows large enough, vision problems may occur due to compression of the optic nerve.
• Suprasellar: Vision problems due to compression of the optic nerves/chiasm.
• Posterior Fossa: Facial symptoms or loss of hearing due to compression of cranial nerves, unsteady gait and problems with coordination.
• Intraventricular: May block the flow of cerebrospinal fluid, resulting in (obstructive hydrocephalus), potentially leading to headaches, lightheadedness and changes in mental function.
• Intraorbital: Buildup of pressure in the eyes, leading to a bulging appearance and potential loss of vision.
• Spinal: Back pain or pain in the limbs caused by compression of the nerves which run into the spinal cord.
Diagnosis
It can be difficult to diagnose meningiomas for several reasons. Because the majority of meningiomas are slow-growing tumors and primarily affect adults, symptoms may be so subtle that the patient and/or doctor may attribute them to the normal signs of aging. Adding to the confusion is that some of the symptoms associated with meningiomas can also be due to other medical conditions. Misdiagnosis is not uncommon and, in fact, may take several years to diagnosis correctly.
When a patient presents slowly increasing signs of mental dysfunction, new seizures or persistent headaches or if there is evidence of pressure inside the skull (e.g. vomiting, swelling of the optic nerve head in the back of the eye), the first step should be a thorough neurological evaluation, followed by radiological studies, if needed.
Sophisticated imaging techniques can help diagnose meningiomas. Diagnostic tools include computed tomography (CT or CAT scan) and magnetic resonance imaging (MRI). Sometimes, the only way to make a definitive diagnosis of the meningioma is through a biopsy. The neurosurgeon performs the biopsy, and the pathologist makes the final diagnosis, determining whether the tumor appears benign or malignant, and grading it accordingly.
Treatment Options
Surgery
Meningiomas primarily are benign tumors, frequently with defined borders and often enabling complete surgical removal, which offers the best chance for a cure. The neurosurgeon opens the skull through a craniotomy to enable full access to the meningioma. The goal of surgery is to remove the meningioma completely, including the fibers that attach it to the coverings of the brain and bone. However, complete removal can carry potential risks that may be significant, especially when the tumor has invaded brain tissue or surrounding veins.
Dr. Robert Jackson utilizes computer assisted stereotactic neuronavigation to assist with the surgical removal of intracranial meningioma. This allows for smaller incisions, less invasive surgery and more complete resections. Length of hospital stay and return to work time are variable based on patient and tumor location factors.
Although the goal of surgery is to remove the tumor, the first priority is to preserve or improve the patient’s neurological functions. With patients for whom total removal of the tumor carries significant risk of morbidity (any side effect that can cause decreased quality of life), it may be better to leave some of the tumor in place and observe future growth with regular imaging studies. In such cases, the patient will be observed over a period of time with regular examinations and MRIs, while for other patients, radiation therapy may be deemed the best approach.
Observation
Observation over a period of time may be the appropriate course of action in patients who meet the following criteria:
- Patients with few symptoms and little or no swelling in the adjacent brain areas
- Patients with mild or minimal symptoms who have a long history of tumors without much negative effect on their quality of life
- Older patients with very slow-progressing symptoms
- Patients for whom treatment carries a significant risk
Radiation Therapy
Radiation therapy uses high-energy X-rays to kill cancer cells and abnormal brain cells, and to shrink tumors. Radiation therapy may be an option if the tumor cannot be treated effectively through surgery.
- Standard External Beam Radiotherapy uses a variety of radiation beams to create a conformal coverage of the tumor while limiting the dose to surrounding normal structures. The risk of long-term radiation injury with modern delivery methods is very low. Newer techniques of delivery aside from 3-dimensional conformal radiotherapy (3DCRT) include intensity-modulated radiotherapy (IMRT).
- Stereotactic Radiosurgery (such as Gamma Knife, Novalis and Cyberknife) is a technique that focuses the radiation with many different beams on the target tissue. This treatment tends to incur less damage to tissues adjacent to the tumor. Currently, there is no data to suggest one delivery system is superior to another in terms of clinical outcome. Each has its advantages and disadvantages.
Chemotherapy
Chemotherapy is rarely used to treat meningioma, except in atypical or malignant subtypes that cannot be adequately treated with surgery and/or radiation therapy.
